In the cervical (neck) and lumbar spine (low back), the vast majority of herniated discs improve with time. This improvement is typically due to over-the-counter pain medications, ice and heat, activity modification, and physical therapy.
The best test for a herniated disc is an MRI scan. X-rays and a myelogram are also sometimes used, but these tests are less commonly ordered. Contact Herniated Disc now!
A herniated disc may cause pain, numbness and weakness in your arms, hands, legs or feet. It can also affect your bladder and bowel. A herniated disk can occur in the lower back (lumbar area), neck (cervical area) or upper-to-mid spine (thoracic area). The most common symptoms of a slipped disc are leg pain, arm pain and back pain. In most cases, herniated discs are not a serious medical condition, but they do require treatment.
Disk herniation usually occurs because of a gradual, age-related wear and tear process in the spinal disks called disk degeneration. This causes the disks to become less flexible, and it is more likely that one of the outer disk edges will slip out of place. Herniation can also be caused by a traumatic event, such as a fall or blow to the back that causes a twist or strain.
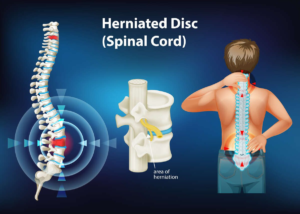
When a herniated disk occurs, the jelly-like center of the disk pushes against the outer disk rings and causes pain in the area where the spinal nerves pass through. The herniated disk material may also cause a chemical irritation of the spinal nerves, which can produce symptoms such as tingling or numbness.
Your doctor will ask about your symptoms and do a physical examination. Your doctor will want to know if your pain goes away when you sit on an exam table and lift your leg straight up, which can help determine where the problem is in the lower back. The doctor may prescribe a pain reliever, muscle relaxant or cortisone injections to reduce the pain and swelling from a herniated disk.
If your herniated disc is in the area of the spine where the nerves that control the bowels and bladder travel, you could have a more serious complication known as cauda equina syndrome. This happens when a large fragment of the ruptured disk herniates into the spinal canal where the nerves that control the bowels go before they leave the spine. This can lead to loss of control over the bowels and bladder, which is a medical emergency.
The backbone, or spine, is made of 26 bones called vertebrae. In between each bone are soft disks that cushion the vertebrae and keep them in place. If a disc ruptures or bulges, it can cause pain and numbness. Your doctor will diagnose a herniated disk with a physical exam and, often, imaging tests. He or she will ask questions about when you first noticed symptoms, what makes them better or worse and where the pain is felt. The location of your pain helps your doctor figure out which nerves are affected by the herniated disc.
Usually, a herniated disk causes pain only in the areas that are served by the involved spinal nerves. Symptoms from herniated discs in the lower back (lumbar spine) are most common, but can occur anywhere in the back or neck (cervical spine). Pain from herniated disks in the upper-to-mid spine is rarer.
A single excessive strain or injury can cause herniated discs, but they also may develop slowly as the outer layer of the disk degenerates over time, allowing the jelly-like center to leak out. Smoking increases your risk of a herniated disk by speeding up the degeneration of the outer disc layers and the nucleus pulposus.
MRI, which uses radio waves and magnetic fields to create detailed images of the spine, can locate the herniated disc and determine its shape and size. It can also show whether the spinal nerves are being compressed by the herniated disk. Your doctor might also use an electromyogram to record the tiny electrical impulses that muscle cells make when they are stimulated. Your doctor can then see whether any nerves are being affected by the herniated disc and its pressure on them.
Herniated discs can lead to a condition called cauda equina syndrome, which occurs when a large fragment of the herniated disk ruptures into the area where the nerves that control your bladder and bowels travel before they leave the spine. This can be very serious and requires surgery to relieve the pressure on the nerves. Even after surgery, there is a 10-15 percent chance that the same disc will herniate again.
A herniated disc can cause pain, but nonsurgical treatment can help. The first step is to reduce activity, if possible, until pain starts to ease. Your doctor will perform a physical exam and ask questions about your pain, weakness and other symptoms. They will check for the location of your pain and how it changes when you move, lift or twist your back. Your doctor may also want to know whether you have trouble with urinating or having bowel movements because this could indicate that the herniated disk is pushing on nerves that control those functions.
Your doctor may order an imaging test to help diagnose a herniated disc. Regular X-rays don’t detect herniated disks, but they can show other causes of back pain such as spinal alignment problems, a tumor, a broken bone or infection. A computed tomography (CT) scan uses a series of X-rays taken from different angles and combines them to create cross-sectional images of your spinal column and the structures around it. This test can find indentations in the spine caused by herniated discs and may reveal bone spurs that might be pressing on your spinal cord or nerves.
An magnetic resonance imaging (MRI) scan is the preferred diagnostic tool for herniated discs. It uses radio waves and a strong magnetic field to create detailed images of the tissues inside your body, including the spinal cord and nerves. MRI can detect indentations in the spinal cord and other tissues that might be causing pain. An interventional radiologist, an expert in pain management procedures, usually performs this test.
Your health care professional might suggest you take pain medicines to control your herniated disk pain. Nonsteroidal anti-inflammatory drugs (NSAIDs) are the most common and are effective in most cases. If these don’t relieve your pain, your doctor might prescribe short-term use of opioid medicines such as oxycodone or an acetaminophen-opioid combination (Percocet). These medicines can make you sleepy and can have serious side effects, including addiction.
If your pain doesn’t respond to nonsurgical treatments, your doctor might consider steroid injections into the area of the herniated disc. NYU Langone pain specialists and radiologists use X-ray guidance to inject the medication into the epidural space, which is the fluid-filled area that surrounds your spinal cord. The injected medicine will reduce swelling around the spinal nerve and might relieve your pain for weeks or months.
There are a number of factors that can affect how quickly you heal from herniated disc. Some of these factors include the severity of your injury, your age, and your overall health. A more severe herniated disc will generally take longer to heal than a less severe one. Your recovery may also depend on your body’s natural ability to heal. Younger people tend to recover from injuries more quickly than older individuals.
Herniated discs can be treated with rest, pain medications and spinal injections. With these treatments, most people feel better within six weeks and are able to return to their normal activities. However, if your symptoms do not improve with these treatments, surgery may be necessary.
If you are diagnosed with a herniated disc, your doctor will conduct a physical exam to determine the source of the pain and test for muscle weakness or numbness. Your doctor will also review your medical history to understand your symptoms and find out what activities seem to trigger your pain.
In most cases, your doctor will recommend that you rest for a few days and then gradually begin your regular activities again. You will be advised to avoid lifting anything over a few pounds, twisting your back at exaggerated angles or partaking in any other activity that could trigger your pain. Your doctor may also advise you to get regular spinal injections that contain a steroid medication. These shots reduce the inflammation in the area of the herniated disc and can control your pain for months at a time.
After you have recovered from your herniated disc, your doctor will recommend that you engage in core exercises to strengthen the muscles that support your spine. This will help to reduce the risk of further herniations in the future. However, if your doctor has recommended that you do core exercises, be sure to only engage in exercises that do not place pressure on the spine. Exercises that involve Russian twists, bending at the waist or bicycle crunches are not a good idea as they can put too much strain on the spine. Instead, do isometric core exercises that are not abrasive on the spine.
